This article is part of our showcase of the 2020 Future of Ageing Awards. SummitCare was awarded highly-commended in the Palliative Care category for its role in implementing the Palliative Care Outcomes Collaboration (PCOC) to improve end of life outcomes at its Smithfield site.
Updated 26th May 2021: Since the original posting further information was supplied by the Palliative Care Outcomes Collaboration (PCOC), which has been added to this story.
Staff from SummitCare achieved greater awareness and understanding of palliative care through the rollout of a national program to improve resident and carer outcomes.
The New South Wales-based aged care provider, which operates 10 homes across Sydney and Newcastle, is implementing the Palliative Care Outcomes Collaboration (PCOC) to improve end of life outcomes at its Smithfield site.
In a submission to Inside Ageing’s Future of Ageing Awards 2021, Corporate General Manager – Sales and Marketing, Rina Fuimaono said the standardised, national approach was being implemented across the service.
“SummitCare supports this project, with the facilitators to implement the PCOC program to enable tools to assess needs, trigger discussions with residents and families for advance care planning and anticipate needs before they arise,” she said.
“It also enables staff to recognise when specialist support, medical or other reviews [are] indicated.”
The Palliative Care Outcomes Collaboration (PCOC) is a national outcomes and benchmarking program with the primary objective of systematically improving palliative care for people who are approaching the end of life, and for their families and carers. PCOC is a collaboration between four Australian Universities (The University of Wollongong, The University of Western Australia, University of Technology Sydney and Queensland University of Technology) and is funded by the Australian Government Department of Health.
The PCOC program involves a protocol for routine clinical assessments to identify the needs of patients and to respond to those needs appropriately. It is now widely used in more than 180 palliative care services across Australia.
PCOC received funding from the J.O. & J.R. Wicking Trust in 2019 to conduct a pilot of the PCOC program in residential aged care. SummitCare, along with several other aged care organisations, partnered with PCOC to pilot the ‘PCOC Wicking Model’ for residential aged care.
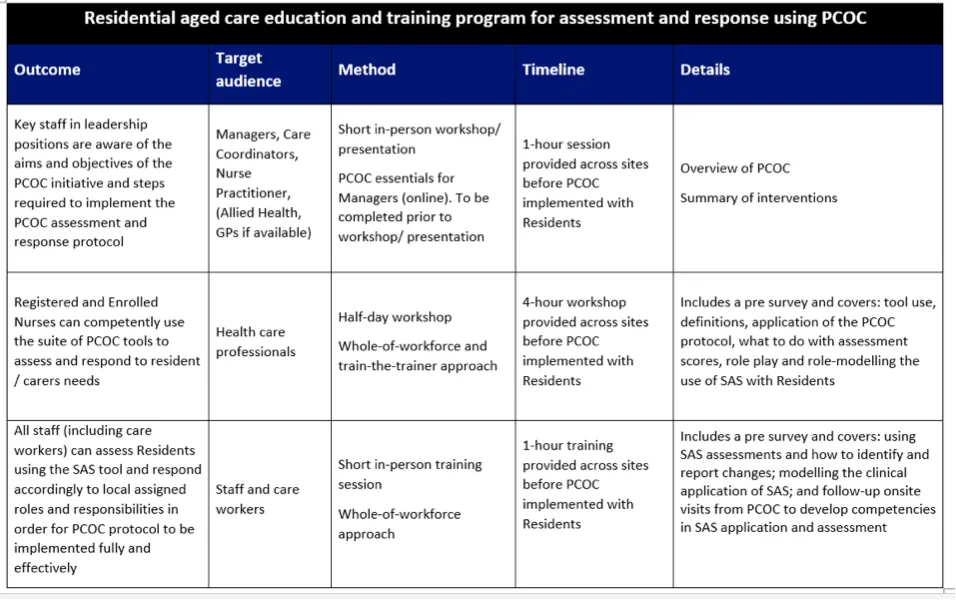
PCOC’s Improvement Facilitators provided training to SummitCare staff at the site involved in the pilot. The PCOC Wicking Model adopts a ‘whole of workforce’ approach in each residential aged care facility (RACF)—recognising the integral role of care workers in monitoring resident’s symptoms and needs. Care workers are trained to monitor residents’ symptoms daily and report changes. Health professionals are trained in the use of the PCOC Wicking assessment and response protocol with each resident. These assessments help inform the appropriate care of residents who are approaching the end of life.
“Part of PCOC’s standardised approach involves the collection of important assessment information (data) for each resident. Every six months data are submitted to PCOC where it will be analysed and reported back to each facility to identify areas for improvement and to drive system-level changes.”
The PCOC Wicking Model recognises that residents’ need for palliative care will change over time. Initially, residents may not require the additional support and monitoring associated with palliative care. The PCOC Wicking Assessment and Response protocol for RAC recommends regular three-monthly screening of residents for the need for palliative care.
Unexpected events such as hospital admission, increasingly frequent falls, if there is significant weight loss or functional changes, or if families raise concerns also prompt re-screening to see if palliative care is appropriate.
Then a palliative care plan can be put in place. Development of a palliative care plan involves talking with the resident and family about their preferred place of care in various circumstances and preferred place of death, consideration of an advanced care plan or ‘not for resuscitation plan’, exploring the nomination of a surrogate decision-maker and reviewing medications with the resident’s general practitioner.
“The implementation of the palliative care plan involves routine assessments using the PCOC measures to ensure residents’ needs are assessed correctly,” the submission said. “The repetition of the measures helps detect any changes in the resident’s needs and ensures they are attended to promptly.”
Leadership staff were engaged in the development of protocols and implementation of the program at SummitCare, with in-person training conducted by PCOC before the program was rolled out. Nurses and all care workers were trained in the use of the PCOC tools.
SummitCare’s submission said the project remains ongoing.
“Being in the pilot has enabled SummitCare Smithfield to identify some issues, then develop and implement improvement activities emphasising how they made a difference to residents receiving palliative care,” the submission said.